Plantar Fasciitis vs Plantar Fasciosis: The Critical Difference Every Patient Must Know
Share
Plantar Fasciitis vs Plantar Fasciosis: Understanding the Critical Difference in Your Heel Pain 🦶✨
As a board-certified podiatrist, I frequently encounter patients who come to me with confusing diagnoses and mixed information about their heel pain. One of the most common sources of confusion? The difference between plantar fasciitis and plantar fasciosis. While these two conditions share similar names and locations, understanding their distinction is absolutely crucial for effective treatment and recovery.
What Makes These Conditions Different? 🔍
The primary distinction between plantar fasciitis and plantar fasciosis lies in the underlying tissue pathology:
Plantar Fasciitis represents the acute, inflammatory phase where your plantar fascia - that thick band of tissue running from your heel to your toes - becomes actively inflamed due to injury or overuse. Think of it as your body's immediate response to tissue damage, complete with swelling, heat, and that characteristic stabbing pain
Plantar Fasciosis, on the other hand, occurs when inflammation has subsided but the tissue has undergone degenerative changes. Instead of active inflammation, you're dealing with scarred, thickened tissue that has lost its normal elasticity and function
The Morning Pain Mystery Explained 🌅
If you've ever wondered why that first step out of bed feels like stepping on broken glass, here's what's happening: During sleep, your plantar fascia naturally contracts and shortens as your foot relaxes. When you suddenly stand up, this tightened tissue gets stretched abruptly, causing those micro-tears to pull apart and create that sharp, intense pain.
This morning stiffness affects both conditions but for different reasons. In plantar fasciitis, it's due to overnight inflammation and reduced blood flow. In plantar fasciosis, the chronically thickened and scarred tissue simply doesn't have the flexibility to accommodate that sudden stretch.
Recognizing Plantar Fasciitis Symptoms 🚨
Plantar fasciitis typically presents with:
-
Sharp, stabbing heel pain that's worst in the morning or after periods of rest
-
Pain that improves with walking as the tissue warms up and stretches
-
Tenderness at the medial calcaneal tubercle (where the fascia attaches to your heel bone)
- Pain that may return after prolonged standing or at the end of an active day
The acute phase typically lasts 4-6 weeks and represents your body's attempt to heal microscopic tears through natural inflammatory processes.
Understanding Plantar Fasciosis Characteristics ⚠️
Plantar fasciosis develops when inflammation fails to resolve properly, usually after 3+ months of symptoms. Key features include:
-
Persistent, dull aching pain that doesn't follow the typical morning pattern
-
Pain that lingers throughout the day rather than improving with activity
-
Presence of heel spurs in some cases (though spurs don't cause the pain)
- Thickened plantar fascia visible on ultrasound imaging
Tissue biopsies in chronic cases show no active inflammation but rather degenerative changes with collagen breakdown and scar tissue formation.
Why the Distinction Matters for Treatment 💊
This isn't just medical semantics - the difference dramatically impacts your treatment approach:
Plantar Fasciitis Treatment (Inflammation Phase)
-
Non-steroidal anti-inflammatory medications (NSAIDs) for pain and swelling relief
-
Ice therapy (ice massage, ice packs)
-
Corticosteroid injections (short-term relief, with risk of heel pad atrophy)
- Rest and modifying activity to reduce stress on the fascia
- Therapeutic ultrasound and phonophoresis
- Physical therapy: manual therapy, stretching, and strengthening exercises
- Kinesiology taping and athletic taping techniques
- Extracorporeal shock wave therapy (ESWT) for recalcitrant cases
- Heel pads or silicone heel cups for cushioning
- Supportive footwear changes and arch supports
- Orthotic devices, especially prefabricated or custom insoles
- Night splints to keep the fascia elongated overnight
- Stretching protocols for the plantar fascia and calf muscles
- Weight management if overweight
- Limited immobilization (e.g., walking boot) for severe cases
Plantar Fasciosis Treatment (Degenerative Phase)
Since there's no active inflammation, anti-inflammatory treatments become less effective. Instead, treatment focuses on:
-
Platelet-rich plasma (PRP) or autologous blood injections to stimulate tissue repair
-
Extracorporeal shock wave therapy (ESWT), often effective in chronic, non-responsive cases
-
Prolotherapy (injecting irritating solutions to promote healing)
- Percutaneous needle tenotomy or microtenotomy (stimulates local healing response)
- Radiofrequency ablation (RFA) for chronic, persistent cases
- Advanced physiotherapy: high-load strengthening exercises for the fascia and intrinsic foot muscles
- Amniotic membrane or stem cell injections (emerging therapies)
- Endoscopic or minimally invasive plantar fascia release (surgery) for recalcitrant cases
- Focused biomechanical correction with orthotics and footwear
- Manual therapy and soft tissue mobilization to address scar tissue and improve flexibility
- Night splints and continued stretching routines
- Dry needling of the fascia
- Gradual return to activity following a period of protected weightbearing
The Role of Footwear and Biomechanics 👟
Inappropriate footwear plays a crucial role in both conditions, but particularly in fasciosis development.
Key footwear recommendations include:
- Shoes that allow your toes to lie flat and spread naturally
- Adequate arch support without excessive heel lift
- Shock-absorbing soles for impact reduction
- Replacement of athletic shoes every 400-500 miles
When to Seek Professional Help 🏥
As a podiatrist, I recommend seeking professional evaluation when:
- Heel pain persists beyond 6-8 weeks despite home treatment
- Pain significantly impacts your daily activities or sleep
- You experience numbering or tingling (which could indicate nerve involvement)
- Your pain pattern changes or worsens over time
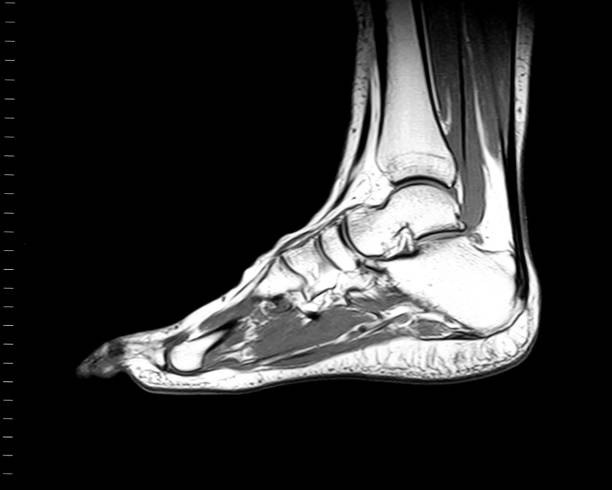
Imaging modalities such as ultrasound or MRI can measure plantar fascia thickness. In healthy individuals this is typically ~2–4 mm (0.2–0.4 cm), while in symptomatic plantar fasciitis it often exceeds 4–5 mm. Thickening combined with changes in echogenicity or signal can suggest degeneration or pathology, though thickness alone cannot reliably distinguish acute from chronic changes.
The Recovery Timeline ⏰
Understanding realistic expectations is crucial:
-
Acute plantar fasciitis: Most cases resolve within 3-6 months with conservative treatment.
- Chronic plantar fasciosis: May require 6-12 months or longer, often needing more aggressive interventions.
Research shows that approximately greater than 90% of patients improve with conservative treatment, but the key is matching the treatment to the correct phase of the condition.
Prevention Strategies That Actually Work 🛡️
Based on current research and clinical experience:
- Daily calf, Achilles tendon, and plantar fascia stretching, especially before the first step in the morning and after long periods of inactivity.
- Gradual progression of exercise intensity and duration to prevent sudden overload of foot structures.
- Weight management to minimize repetitive stress and lower the risk of developing heel pain.
- Choosing supportive shoes with proper arch support, shock absorption, and a comfortable fit; replacing athletic footwear regularly to ensure optimal cushioning.
- Early identification and correction of abnormal foot biomechanics (e.g., flat feet or high arches) using custom orthotics or insoles when needed.
- Incorporating foot-strengthening exercises to enhance intrinsic muscle stability and improve shock absorption capacity.
- Applying athletic or kinesiology tape if planning intensive activities or during symptom flare-ups to offload the plantar fascia.
- Avoiding prolonged barefoot walking on hard surfaces, especially on tile, hardwood, or concrete floors.
- Taking regular standing or walking breaks throughout the day and alternating between sitting and standing, especially for individuals with sedentary or standing occupations.
- Using myofascial release techniques, such as rolling a ball or frozen water bottle under the arch, to help maintain fascia flexibility and decrease tissue tightness.
- Monitoring training surfaces: opting for softer, even surfaces and alternating running or walking routes to reduce repetitive stress.
- Managing other medical conditions that alter gait mechanics, such as arthritis, to prevent compensatory overloading of the heel.
- Seeking early podiatric evaluation for persistent or recurring heel pain to address risk factors before the condition becomes chronic.
These strategies, supported by clinical research and podiatric guidelines, can significantly lower the risk of both inflammation-driven and chronic degenerative heel pain.
The Bottom Line ✅
While plantar fasciitis and plantar fasciosis may sound similar, they represent different stages of the same disease process. Fasciitis involves active inflammation and responds well to anti-inflammatory treatments, while fasciosis represents chronic degeneration requiring regenerative and mechanical interventions.
The good news? With proper diagnosis and appropriate treatment, both conditions are highly treatable. The key is understanding which phase you're experiencing and matching your treatment accordingly.
If you're dealing with persistent heel pain, don't assume it's "just" plantar fasciitis. Getting an accurate diagnosis from a qualified podiatrist can make the difference between months of ineffective treatment and a targeted approach that gets you back to pain-free walking.
Remember, your feet carry you through life - they deserve the best care possible! 🦶💪
Dr. Ahmad Rashid, DPM
Board-Certified Podiatrist & Founder, PodiatryMarket.com
Disclaimer: This post is educational and not intended as a substitute for medical advice. Consult your healthcare professional for personalized recommendations.
